Improving Population Health
According to CMS, the U.S. healthcare system spends $10,3481 per person every year (highest in the world) to manage, track, analyze and carry out care coordination and quality improvement initiatives. Six in ten Americans live with at least one chronic disease, like heart disease, cancer, stroke, or diabetes2. These and other chronic diseases are attributed to be the major reasons of death and disability in America, and prominent drivers of health care costs.
According to a famous RAND study, American adults receive recommended care only 55 percent of the time 3. The gaps in treatment lead to avoidable complications, ER visits, and hospitalizations — a major component of the waste in the system. Additionally, understanding and managing patient risks is a huge problem for population health today
Evolving healthcare policies and rise in consumerism place a heavy burden on organizations to improve patient care outcomes, while reengineering patient engagement.
Putting PHM to work
As the industry continues its transition from volume-based to value-based healthcare, it is important to proactively identify population segments that are in need of care as well as apply differential and relevant care strategies for patients while also focusing on reducing costs, improving experiences and driving appropriate utilization.
The pivot for success in this new value-care-driven ecosystem is maintenance or improvement of patient’s health and reduction in cost of care. The way forward is managing population health effectively and efficiently.
Population health management (PHM) programs are key to clinical and financial success under value-based care delivery models. It begins with risk stratification of the population to identify patients who have the greatest health risks (therefore, pose financial risks to the organization).
PHM requires a high degree of intelligent automation to assess and reach everyone in the population, engage patients in self‐care, and maximize the chances of each person receiving proper preventive, chronic, and acute care when needed. The health system needs vendors who can deliver a comprehensive solution that unifies data, analytics, and services.
The 4 broad pillar of PHM program are:
- Member Stratifications: The purpose of stratification is identifying members based on the risk that they carry, for e.g. complex care (multiple comorbid conditions). These patients can then be targeted and care can be delivered effectively.
- Performance Reporting: The healthcare system needs an efficient performance management framework to track performance against industry programs such as ACO, MIPS Star, etc., and help analyze care delivered at the individual patient level.
- Care Gap Management: Using a unified care management solution, payers and providers can collaborate to improve the health of the patient by closing any identified care gaps. Timely closure of gaps leads to healthy patients and improved financial reimbursements.
- Member Engagement: 80% of a member’s health is dependent on non-clinical factors. By employing personalized engagement strategies, members can be empowered to get invested in taking care of their own health.
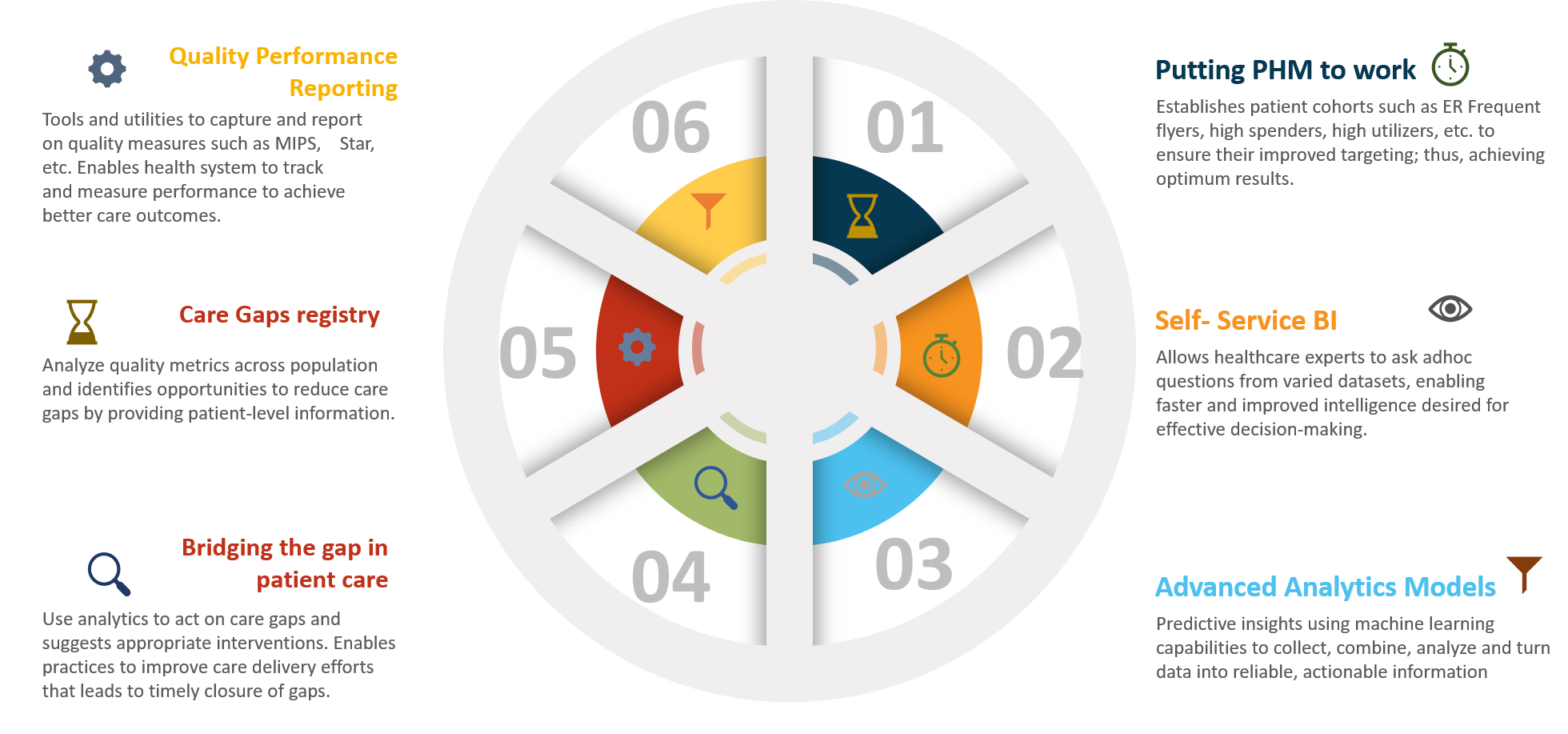
How ITC Infotech can help!
ITC Infotech’s ‘Healthcare Insights’ is a big data analytics platform that supports population health initiatives. It helps healthcare organizations measure and track performance of services delivered. It leverages machine learning to predict performance and patients who are likely to not receive optimal care.
With nearly a decade’s experience in working with healthcare organizations globally, ITC Infotech has developed significant experience in helping payers and providers improve quality of care delivered, care coordination and engagement. We bring our strong consulting skills and technology expertise supported by pre-built analytical assets. The combination makes ITC Infotech the preferred strategic partner for advisory, data analytics and information management the world over.
Healthcare Insights – Improving Patient Outcomes